philosophy | ecology | pathobiology | immunology | neurobiology
Who is Jackie Howells?
As an ecologist and immunologist by training, one of the most important inquiries of modern biomedical science that endlessly fuels my curiosity is how physiological systems influence one another. It is becoming increasingly clear that Investigations of how physiological systems interact are imperative to understanding fundamental mechanisms of disease pathogenesis and is key to unlocking novel targeted therapies.
As an ecologist and immunologist by training, one of the most important inquiries of modern biomedical science that endlessly fuels my curiosity is how physiological systems influence one another. It is becoming increasingly clear that Investigations of how physiological systems interact are imperative to understanding fundamental mechanisms of disease pathogenesis and is key to unlocking novel targeted therapies.
Ecoimmunology perspective.
Many other immune cells have been used for cellular immunotherapy, in combination with monoclonal antibody therapy, to harness the immune system in a targeted way. Some of the most famous of which are based on manipulating T cells to kill cancers of the blood. When considering any immunotherapy it is crucial to determine parameters, both internal (endogenous) and external (exogenous) to properly diagnose patients in the clinic, effectively determine mechanism of pathogenesis, and from basic research in the lab synthesized with epidemiological and ecological data collected, determine what intervention, whether that be external, internal, or behavioral is required to reduce the most suffering.
Exploring Education: How can we harness unique perspectives to learn and teach effectively & efficiently?
”To learn easily is naturally pleasant to all people, and words signify something, so whatever words create knowledge are the pleasantest. . . .”- Aristotle
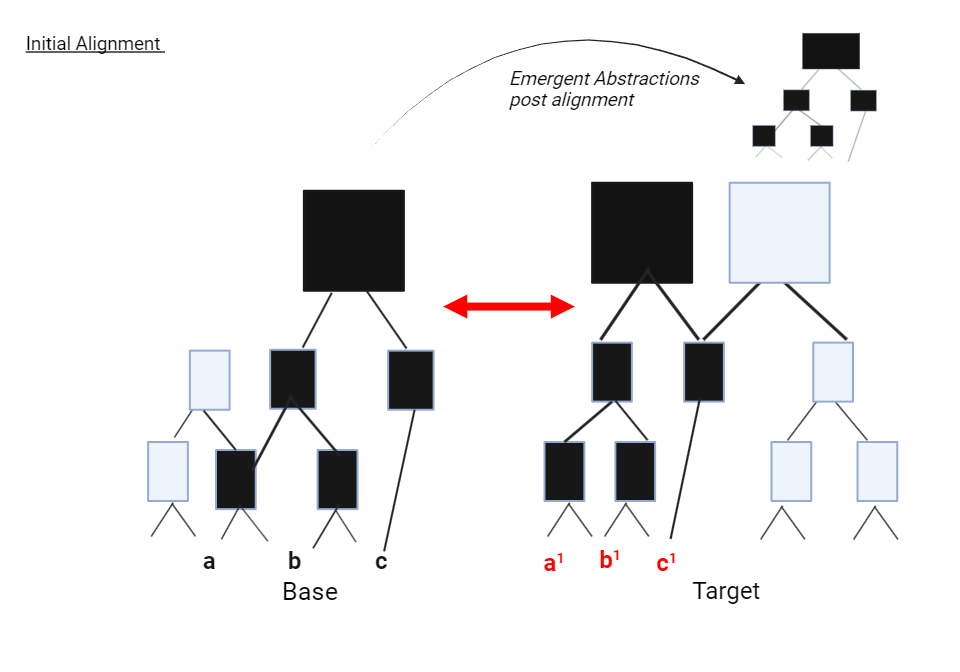
I am currently working on a project that is dear to my heart as a lover of language and playing with words wiht metaphor as a mechanism of teaching in jargon heavy fields. We can rely on our increased semantics from unique individuals within our population to foster quality scientific inquiry which is transmissible from the base to the target.



Progenitors at the organ cellular and subcellular levels.
In my PhD research and since I have been fascinated by neutrophil biology and the mechanisms underlying this elusive cell’s contributions to health and disease. Neutrophils have often been considered to be the “fast and dirty” innate immune cells who are the first to arrive at a site of injury to prevent infection. Neutrophils have fascinating kinetic and physical properties including their ability to roll across tissue, use slings and tethers to stop at a particular spot, and are able to cast neutrophil extracellular traps(NETs) to trap large microbes like fungi. Given these many properties I am very interested in probing their capability of immunomodulation and excited to see what we find in the Lefort Lab
Journalism & Writing
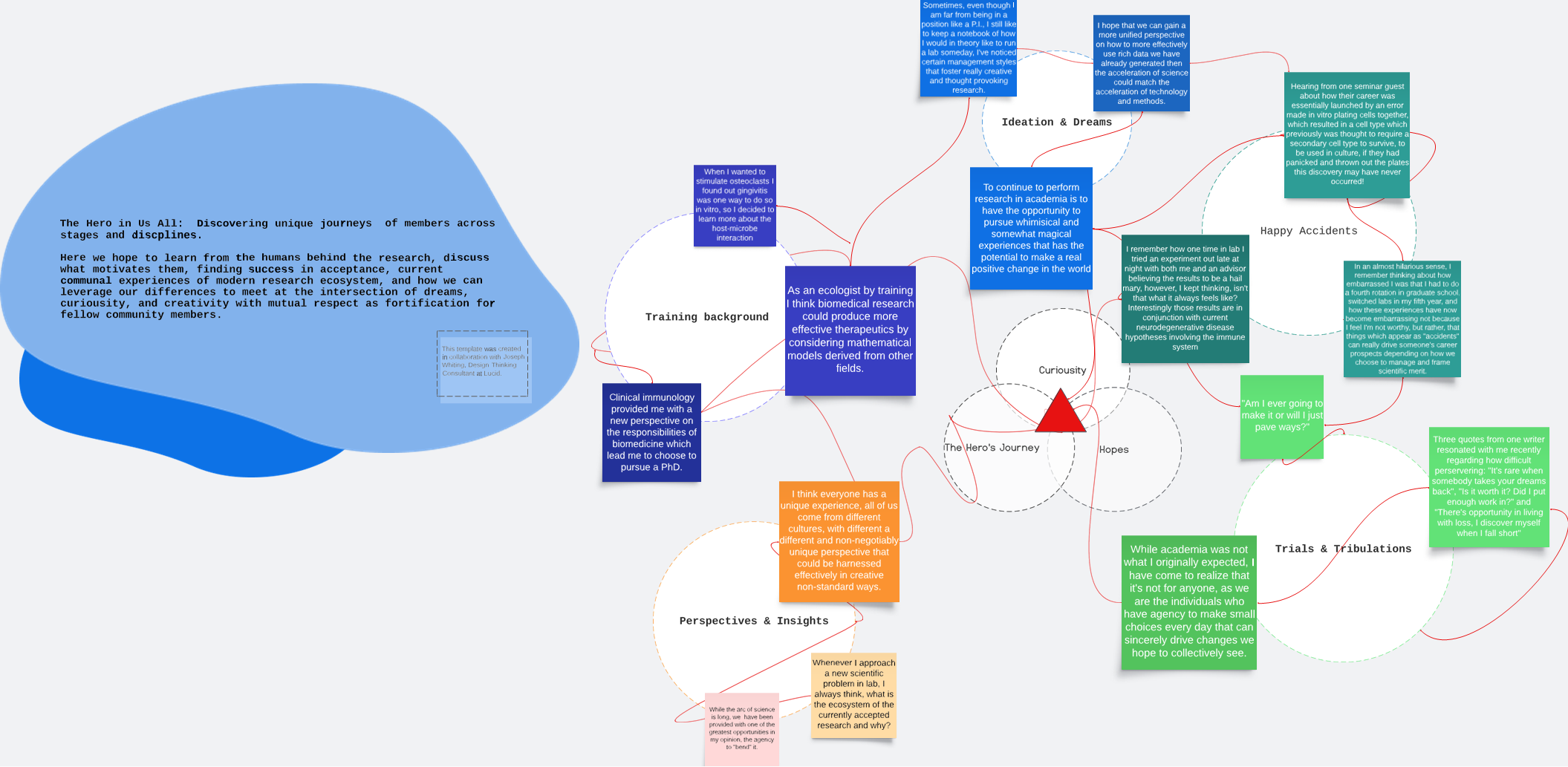
I am currently exploring journalism through a newsletter series entitled: The Hero’s Journey in collaboration and supported by the Society of Leukocyte Biology. This endeavor has been such a hopeful one as I spoke for 30min-2 hours with members across various domains and levels of career stage via online meetings with nearly 20 scientists at trainee, early career, middle career, and senior leaders in their fields. I think the more we communicate openly about what our journey looks like and who we are as people, has compelled me far more than any graph or publication alone to continue to advocate for science as a true value to the world and ecosystems as we all iteratively learn. This story strings map was created during my ideating phase of determining: what makes a hero?
Engraftment of neutrophil progenitor cells in bone marrow.
My PhD dissertation investigated a neutrophil progenitor cell line derived from HOXB8 progenitors which are unique in their ability to engraft in unconditioned bone marrow. Typically for stem cell transplant for myeloid derived diseases such as acute myeloid leukemia, cancerous cells must be eliminated via chemotherapy or irradiation. This process also creates required space in the bone marrow for transplanted cells to home and engraft into. In 2022, Cohen et al. published a study from the Lefort lab entitled Engraftment, Fate, and Function of HoxB8-Conditional Neutrophil Progenitors in the Unconditioned Murine Host”
Interacting Modalities: population immunology & therapeutics
The potential for any immunotherapy under an ecoimmunology framework requires systems interactions across trophic levels and between populations and individuals within groups and between to provide comprehensive care for our fellow humans.
Neutrophil potential in cellular therapeutics for diseases stemming from neutrophil dysfunction such as congenital chronic granuloma disease, have remained technically unfeasible until recently engineered conditionally immortalized neutrophil progenitor cells were created as described in Wang et al.’s publication: “ Quantitative production of macrophages or neutrophils ex vivo using conditional Hoxb8” in 2006. ( Wang, Gang G., et al. "Quantitative production of macrophages or neutrophils ex vivo using conditional Hoxb8." Nature methods 3.4 (2006): 287-293.) Since, this novel tool has provided an avenue to pursue researching cellular therapeutic potential of neutrophils, which are normally difficult to study as they are short lived (only two days) and are post mitotic, meaning they don’t divide further in vitro culture making it incredibly difficult to produce enough cells from the body to perform experiments required for genomic manipulation or expansion for transplant.
(https://doi.org/10.3389/fcell.2022.840894) demonstrating a line of HoxB8 progenitors which could engraft in bone marrow prior any cytoreductive conditioning, and which were fated to mature into functional neutrophills capable of killing bacteria.
“From the bottom of my heart thanks to all who were instrumental to my PhD success!!! I am so grateful for every individual in this photo and so lucky to have them take the time and consideration as my mentors and peers to spend different parts of my 7 year scientific pathobiology odyssey! Will update soon! ”
The Neutrophil and potential therapeutic avenues.
I am currently continuing this work to determine the mechanisms underlying this cell line’s engraftment in addition to their potential therapeutic use under chemotherapeutic conditioning. Our idea is that this cell line might be useful as an adjunct therapy to chemotherapy, which leaves the patient without an immune system to fight infection until their immune system repopulates. We propose that providing patients with neutrophil progenitors may provide a transient protection for patients against infections while their own immune system repopulates.
Thank you so much to the Society of Leukocyte Biology & the Journal of Leukocyte Biology in addition to my mentor Dr. Craig Lefort for introducing me to the society to have an opportunity to share my work in 2022 in Mexico City at “The Neutrophil” conference (yes there’s a whole conference!)
Tau mediated neurodegeneration
Prior to this project, during my PhD I investigated the complex relationship between the immune and nervous system using drosophila as a model organism. Many very exciting studies have been recently published under the umbrella of the “Antimicrobial Peptide Theory of Neurodegeneration” put forth by Dr. Moir and Dr. Tanzi. Learning how model organisms like drosophila can be used as such a powerful genetic tool to map immune pathways, neuronal circuitry, neurobiological changes, and behavior has been an important aspect of learning more about how basic and translational science meet. The questions I find most compelling is how perturbations to either of these systems contribute to the pathogenesis neurological disorders. I am particularly interested in how the innate immune system regulates neuronal function, behavior, memory, and in the pathogenesis of neurodegenerative disease. This is also a very exciting time to work on the immunology of the nervous system given that until very recently (even when I started graduate school in 2017) many still believed that the brain didn’t have a complex immune system or that the system was isolated from the rest of the body so much so that resident immune cells in the brain and peripheral nervous system have been yet to be broadly characterized. Even more interesting is what concepts will emerge from this work which begin to probe the interactions between the nervous system and it’s unique characteristics with the immune system. How does a firing neuron, for example, shape the behavior of an immune cell and vice versa? How does each system regulate the other? What will this tell us regarding behavioral choices we can make to regulate our nervous system that may impact our immune system to increase overall health? These fields are completely open and I’m excited to be able to have access to these studies to elucidate these fascinating interactions. My ultimate goal is to better characterize and understand the mechanisms of disease pathogenesis in order to develop better therapies and reduce human suffering.
Asking the real questions
(jk just asking questions forever)
The more that I learn, the more questions I have. I delight in conversations with others and finding the similarities between dissimilarities.
A subaim of reducing human suffering (my main and consistent value throughout life as a human being myself) is to imbue onto others what has been afforded to me: the comfortability of asking anyone any question and feeling excited for such discussion.
I know I’ve learned from every individual I’ve encountered. Learning how to learn uniquely is a special special process that everyone should be acknowledged for and celebrated.
ORIGINAL FRONT PAGE!
In my PhD research and since I have been fascinated by neutrophil biology and the mechanisms underlying this elusive cell’s contributions to health and disease. Neutrophils have often been considered to be the “fast and dirty” innate immune cells who are the first to arrive at a site of injury to prevent infection. Neutrophils have fascinating kinetic and physical properties including their ability to roll across tissue, use slings and tethers to stop at a particular spot, and are able to cast neutrophil extracellular traps(NETs) to trap large microbes like fungi. Given these many properties I am very interested in probing their capability of immunomodulation and excited to see what we find in the Lefort Lab. Many other immune cells have been used for cellular immunotherapy, in combination with monoclonal antibody therapy, to harness the immune system in a targeted way. Some of the most famous of which are based on manipulating T cells to kill cancers of the blood. Neutrophil potential in cellular therapeutics for diseases stemming from neutrophil dysfunction such as congenital chronic granuloma disease, have remained technically unfeasible until recently engineered conditionally immortalized neutrophil progenitor cells were created as described in Wang et al.’s publication: “ Quantitative production of macrophages or neutrophils ex vivo using conditional Hoxb8” in 2006. ( Wang, Gang G., et al. "Quantitative production of macrophages or neutrophils ex vivo using conditional Hoxb8." Nature methods 3.4 (2006): 287-293.) Since, this novel tool has provided an avenue to pursue researching cellular therapeutic potential of neutrophils, which are normally difficult to study as they are short lived (only two days) and are post mitotic, meaning they don’t divide further in vitro culture making it incredibly difficult to produce enough cells from the body to perform experiments required for genomic manipulation or expansion for transplant. Currently I am investigating a neutrophil progenitor cell line derived from HOXB8 progenitors which are unique in their ability to engraft in unconditioned bone marrow. Typically for stem cell transplant for myeloid derived diseases such as acute myeloid leukemia, cancerous cells must be eliminated via chemotherapy or irradiation. This process also creates required space in the bone marrow for transplanted cells to home and engraft into. In 2022, Cohen et al. published a study from the Lefort lab entitled Engraftment, Fate, and Function of HoxB8-Conditional Neutrophil Progenitors in the Unconditioned Murine Host” ( https://doi.org/10.3389/fcell.2022.840894) demonstrating a line of HoxB8 progenitors which could engraft in bone marrow prior any cytoreductive conditioning, and which were fated to mature into functional neutrophills capable of killing bacteria. I am currently continuing this work to determine the mechanisms underlying this cell line’s engraftment in addition to their potential therapeutic use under chemotherapeutic conditioning. Our idea is that this cell line might be useful as an adjunct therapy to chemotherapy, which leaves the patient without an immune system to fight infection until their immune system repopulates. We propose that providing patients with neutrophil progenitors may provide a transient protection for patients against infections while their own immune system repopulates.
Prior to this project, during my PhD I investigated the complex relationship between the immune and nervous system using drosophila as a model organism. Many very exciting studies have been recently published under the umbrella of the “Antimicrobial Peptide Theory of Neurodegeneration” put forth by Dr. Moir and Dr. Tanzi. Learning how model organisms like drosophila can be used as such a powerful genetic tool to map immune pathways, neuronal circuitry, neurobiological changes, and behavior has been an important aspect of learning more about how basic and translational science meet. The questions I find most compelling is how perturbations to either of these systems contribute to the pathogenesis neurological disorders. I am particularly interested in how the innate immune system regulates neuronal function, behavior, memory, and in the pathogenesis of neurodegenerative disease. This is also a very exciting time to work on the immunology of the nervous system given that until very recently (even when I started graduate school in 2017) many still believed that the brain didn’t have a complex immune system or that the system was isolated from the rest of the body so much so that resident immune cells in the brain and peripheral nervous system have been yet to be broadly characterized. Even more interesting is what concepts will emerge from this work which begin to probe the interactions between the nervous system and it’s unique characteristics with the immune system. How does a firing neuron, for example, shape the behavior of an immune cell and vice versa? How does each system regulate the other? What will this tell us regarding behavioral choices we can make to regulate our nervous system that may impact our immune system to increase overall health? These fields are completely open and I’m excited to be able to have access to these studies to elucidate these fascinating interactions. My ultimate goal is to better characterize and understand the mechanisms of disease pathogenesis in order to develop better therapies and reduce human suffering.
Outside of my research interests, I have a strong passion for building a supportive graduate school community through peer mentorship. Working with students in the Pathobiology program at Brown, we have developed a strong mentorship program dedicated to promoting and improving graduate student well-being. Our mission is to foster supportive relationships with fellow graduate students through community-building activities, regular communication, and personalized mentorship. In recognition of the benefits of maintaining a healthy, engaging academic life for both personal and professional productivity, the goal of the mentorship program is to cultivate meaningful community and interpersonal relationships.